You are viewing the old version of our office blog. Our current blog is located here.
The Holistic Dentist Blog Has Moved
Comments Off on The Holistic Dentist Blog Has Moved
Filed under Biological Dentistry
5 Facets of a Healthy Lifestyle
Repost
We all say we want to be “healthy,” but what does that mean? Is “health” just the absence of illness? If so, then there are a lot of unhealthy people here in the US, where almost half of all adults have at least one chronic disease. In fact, continues the CDC, 70% of all deaths each year are caused by such diseases, especially heart disease, cancer and stroke.
The picture isn’t much prettier globally. Noting that 36 million people died from these kinds of diseases in 2008, the UN predicts that number to rise to 52 million within two decades, eclipsing deaths from “communicable, maternal, perinatal and nutritional diseases.”
But here’s the most distressing thing: these diseases are largely preventable. What we put into our bodies and how we use them have a big impact on whether (and how) we get sick.
In this light, health is less a state of being than a way of being.
A while back, the American Heart Association ran a health views survey of young adults. According to the LA Times, most participants “said they felt they were living a healthy lifestyle.” The youngest (ages 18 to 24) “strongly claimed that living a long, healthy life was important to them. On average, they said they wanted to live until age 98.” Yet 1/3 said that “they don’t believe that doing healthy things now…will make any difference….”
Maybe one of the problems is that we don’t really know what we’re talking about when we talk about “health.” Just what is a “healthy lifestyle”? How could anyone ever achieve it if they don’t know what it is?
The Wholeness of Health
As a holistic dentist, I take a “whole-body” approach to dentistry, treating the teeth and gums in their relationship with the rest of the body. Simply put, oral health affects systemic (overall) health, and vice versa. Likewise, physical health can’t be treated as something severed from our mental life. What happens to us physically also affects “how we feel inside,” and mental states can manifest physically – for instance, a headache or stomachache when you’re anxious or stressed.
Everything is connected. So it’s not hard to see how “living healthy” both involves the whole person and benefits the whole person – body, mind and spirit.
Below are 5 key facets of a healthy lifestyle. While acting on them is no guarantee of perfect health, it can dramatically lower your overall disease risk.
5 Facets of a Healthy Lifestyle
- Good diet/nutrition – A good diet is based on whole foods, including lots of vegetables, fruits and whole grains. It’s low in added sugars and other refined carbohydrates. Junk foods are a rare indulgence, if eaten at all.
- Physical activity – Though most of us lead sedentary lives, this inertia isn’t normal. We evolved to move. Regular exercise and physical activity are a must.
- Avoiding toxins – No tobacco. No drugs. Alcohol in moderation. Minimize exposure to toxic chemicals as you are able. (See EWG’s Healthy Home Tips to learn how.)
- Rest & sleep – Constant “busy-ness” is a surefire recipe for burnout. We need time off – for fun, for relaxation, for simply being. Getting enough quality sleep also matters, since that’s when our bodies do most of their repair work (e.g., rebuilding muscle, consolidating memory).
- Nurturing mental & spiritual well-being – Our overall sense of wellness is enhanced when we give time to ourselves, our loved ones and the things that interest us and give our lives meaning. We find emotional fulfillment. We keep our lives in balance. And this supports our physical well-being.
Modified from the original.
Filed under General Health, Wellness
Oral Cancer: To Screen or Not to Screen?
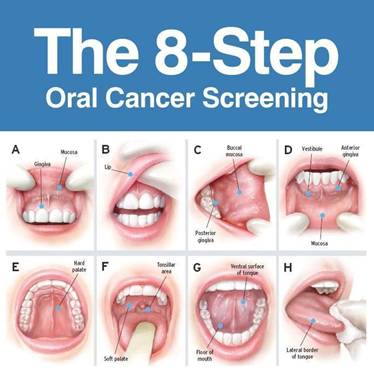
April is Oral Cancer Awareness Month, and this year, it’s involved some controversy.
It began with the release of a Consumer Reports article that included oral cancer screening among 8 “to avoid.”
“Most people,” they wrote, “don’t need the test unless they are at high risk, because the cancer is relatively uncommon.”
Not long after, a government task force said “that there is not enough published evidence to recommend for or against screening for oral cancer by primary care professionals.” Though dentists aren’t considered “primary care professionals” in this case, it’s an easy detail to miss.
So is CR right about when they say such testing isn’t necessary?
While it’s true that oral cancer used to be rather rare, with mostly smokers and heavy drinkers being at risk, that’s no longer the case. As we’ve noted before, rates have been skyrocketing, largely due to the human papillomavirus, or HPV. More than 35,000 new cases are diagnosed each year, and the 5 year survival rate is only 50%. Part of the reason for that last statistic is that many oral cancers are detected quite late – which is why dentists have been speaking up more and more about the benefits of early detection.
Unlike many other kinds of cancer screening, a screen for oral cancer is hardly invasive. At minimum, it involves a visual exam that can quickly and easily be done as part of a routine dental exam.
Many also use technology to aid to visual screening. In our office, we have a device called VelScope, which uses a blue excitation light to make healthy areas appear fluorescent and problem areas, dark. This isn’t some extra procedure; once a year, it’s a part of every adult patient’s exam.
Brian Hill, executive director of the Oral Cancer Foundation, nicely sums up the case for screening:
It isn’t an invasive exam, there’s no radiation (no long-term exposure issue), it is painless, it’s usually free, and you’re already sitting in the dentist chair. Why would you not get it?
Indeed.
Filed under Oral Health
Sugar & the Modern Food Environment (Guest Post)
From the blog of Dr. Bill Glaros – Used with permission
Sugar has one thing going for it: It makes things taste good. And it’s a taste we’re born to prefer.
In the natural settings that human primate ancestors evolved in, sweetness intensity should indicate energy density, while bitterness tends to indicate toxicity. The high sweetness detection threshold and low bitterness detection threshold would have predisposed our primate ancestors to seek out sweet-tasting (and energy-dense) foods and avoid bitter-tasting foods. Even amongst leaf-eating primates, there is a tendency to prefer immature leaves, which tend to be higher in protein and lower in fibre and poisons than mature leaves. The “sweet tooth” thus has an ancient evolutionary heritage, and while food processing has changed consumption patterns, human physiology remains largely unchanged.
And therein lies the problem. Food and beverage manufacturers bank on this preference: Sweet sells, and we pay. The average American diet is so sugared up, we now eat over a hundred pounds of added sugars each year – roughly double what we ate a century ago. And what have we gotten for it? Not much nutrition but lots more obesity and illness. As Dr. Robert Lustig noted in his widely read and commented upon article in Nature earlier this year,
Authorities consider sugar as ’empty calories’ – but there is nothing empty about these calories. A growing body of scientific evidence is showing that fructose can trigger processes that lead to liver toxicity and a host of other chronic diseases. A little is not a problem, but a lot kills – slowly….
Is it really coincidence that industry front groups have been putting out more pro-sugar messages than usual? The month after publication of Lustig’s article, the International Food Information Council added a “Sugars and Health Resource Page” to pound home the point of how wholesome, safe and healthy sugar can be.
More recently, the New England Journal of Medicine published a set of articles on a major source of sugar: soft drinks. As noted in the lead editorial,
Sugar intake from sugar-sweetened beverages alone, which are the largest single caloric food source in the United States, approaches 15% of the daily caloric intake in several population groups. Adolescent boys in the United States consume an average of 357 kcal of the beverages per day….
Unlike carbohydrates with high fiber content, sugar-sweetened beverages are nutrient-poor and are often associated with consumption of salty foods and fast foods. An emerging association between the increased consumption of sugar-sweetened beverages and chronic diseases such as type 2 diabetes, hypertension, and coronary heart disease is a major concern.
Before the end of the day, the beverage industry was in full spin mode, tossing out unreferenced “facts” that largely sidestep the issues at hand. That “forty-eight percent of overweight and obese individuals drink no sugar-sweetened beverages” says nothing about those who do. And while it’s true that sugary drinks aren’t the sole source of increased caloric intake, they still play a role (in all their super-sized glory).
More, soft drinks offer nothing nutritionally – one reason why they’ve become an easy target for regulation. With processed food, you still get some nutritional value with the junk. With soft drinks, you get nothing but colored sugar water with some preservatives (and maybe a vitamin or two thrown in if it’s an “energy” or “smart” drink).
And it’s not just about the sugar. Too often, junk foods and soft drinks replace real, nutrient-dense foods. The fuller we get on that highly processed stuff, the less we eat things like vegetables and whole fruit. That displacement, in fact, may play a crucial role in the health damage we see from sugar-intensive diets. As Dr. Weston Price wrote in Nutrition and Physical Degeneration,
There is very little of the body building minerals in maple syrup, cane syrup from sugar, or honey. They can all defeat an otherwise efficient [healthy diet]. The problem is not so simple as merely cutting down or eliminating sugars and white flour, though this is exceedingly important. It is also necessary that adequate mineral and vitamin carrying foods be made available [to the body].
But sugar is so nice! you say. Indeed, it is – and even nicer when used less often and in smaller amounts. Here are 12 great tips from Mother Nature News to help get you started.
Image by kaibara87, via Flickr
Filed under Diet & Nutrition
Dr. David Kennedy’s Fluoridegate
A new documentary well worth your time and attention, from one of America’s leading experts on fluoride and fluoridation:
Amalgams & Mercury Damage
 Before yesterday was through, the ADA was in full spin mode over Thursday’s Dr. Oz Show: “Are Your Silver Fillings Making You Sick?” Apparently oblivious to irony, they reiterated their usual claim that there’s “no sound science” supporting mercury amalgam’s well-documented health risks – and then insisted on its safety.
Before yesterday was through, the ADA was in full spin mode over Thursday’s Dr. Oz Show: “Are Your Silver Fillings Making You Sick?” Apparently oblivious to irony, they reiterated their usual claim that there’s “no sound science” supporting mercury amalgam’s well-documented health risks – and then insisted on its safety.
As if saying something often and loudly and forcefully enough could somehow make it true.
It’s like when amalgam’s defenders say that the mercury it contains isn’t the dangerous kind – and is even a little magical:
Mercury is an important component in the fillings because it effectively binds the other metals together, forming a strong bond that contributes to the filling’s durability. It is important to note that there are several kinds of mercury. The mercury found in water that can build up in fish and lead to health problems if you ingest too much is not the same type of mercury used in amalgam. The mercury in amalgam is contained, or sequestered, within the filling.
Of course, even the ADA agrees that mercury vapor is released during chewing or grinding. A 2009 paper in Chemical Research in Toxicology estimated that older fillings may have lost up to 95% of their original mercury content. That mercury doesn’t just disappear, of course. The body’s self-regulating mechanisms clear as much of it as it possibly can. That which isn’t excreted is stored, typically gravitating toward fatty tissues such as the liver and brain.
More, although the mercury in amalgam may start out in elemental form, it doesn’t stay that way. As Dr. Huggins notes in It’s All in Your Head, mercury released from amalgams fillings can become methylated.
Mercury is highly reactive chemically. It likes to combine with biological tissue. In the mouth, mercury has the ability to combine with a carbon-hydrogen compound called a methyl group. When mercury combines with methyl groups it is called methyl mercury.
Methylation actually begins in the mouth , due to the action of oral bacteria, but it can occur elsewhere (also). And “although the amounts found are small,” wrote researchers in the Journal of Nutritional & Environmental Science, “any measurable amount of methyl mercury” only adds to a body’s total toxic burden.
Methylmercury is a bioaccumulative toxin. That’s why mercury in fish – especially fatty fish – is such a concern. When mercury contaminates water, it gets methylated by bacteria. Fish exposed to this methylmercury accumulate it in their bodies. When we eat them, we get a dose of the stuff, too.
And there is no question about it: the stuff is highly toxic. It’s main damage is neurological, particularly during the developmental period before birth and into a child’s early years of life.
Of course, it has other effects, as well – including a somewhat surprising one suggested by a recent study. Methylmercury exposure in young adulthood appears to raise the risk of developing diabetes later in life.
The study, published last month in Diabetes Care, analyzed data from nearly 4000 adults between the ages of 20 and 32. According to lead author Ka He of Indiana University,
Our results are consistent with findings from laboratory studies and provide longitudinal human data, suggesting that people with high mercury exposure in young adulthood may have elevated risk of diabetes later in life.
Why? It may be related, at least partly, to pancreatic beta cell dysfunction. These cells have been shown to play a major role in type 2 diabetes.
The abstract of the Diabetes Care study is available here.
We know that our current diabetes epidemic, like its companion obesity epidemic, has many causes. Further study is needed to know if we need to add yet another cause to that list.
Image by Enzo Carretta, via Wikimedia Commons
Filed under Mercury
Bad Breath? Good News!
If you decide what to read on the basis of whether or not it has a catchy title, you likely missed “The Efficacy of Different Mouthrinse Formulation in Reducing Oral Malodour: A Randomized Trial” in the Journal of Clinical Periodontology (presuming, of course, you’re the type who reads things like the Journal of Clinical Periodontology).
 So let’s call it “How Well Do Different Mouthwashes Get Rid of Stinky Breath?” instead.
So let’s call it “How Well Do Different Mouthwashes Get Rid of Stinky Breath?” instead.
Are you interested now?
The randomized, double-blind trial was small and simple: For one week, 18 participants used one of three rinses. Two products – Halita and Meridol with zinc lactate – contained at least one antimicrobial agent (Halita contains cetylpyridinium chloride and chlorhexidine in addition to the zinc). The other contained fluoride.
Sulfur levels and organoleptic (“sniff test”) scores were taken twice to measure odor – once 15 minutes after their first rinse and again at the end of the week. The first took note of masking effects, while the second noted therapeutic effects.
Those were the rules, but how did it turn out?
All three rinses did fine with respect to immediate freshness, but only those with antimicrobials showed a therapeutic effect. They also had the most powerful masking effect.
Does this mean chemical clean is the way to go?
All have their downsides. Chlorhexidine and cetylpyridinium chloride tend to stain the teeth. The latter may also irritate the soft tissues of the mouth or trigger allergic reactions. Fluoride, of course, has its own problems.
And none have proven much better than more natural products, which raises the issue we’ve noted before:
If the effects of natural substances on oral [pathogens] are at least as good as those of a chemical substance, why opt for the chemical?
One alternative we especially like is Natural Dentist Healthy Gums Mouth Rinse. This natural mouthwash helps control periodontal disease and biofilm (plaque) build-up through its blend of cleansing and soothing botanicals including echinacea, golden seal, grapefruit seed, aloe vera gel and calendula. It contains no alcohol, artificial sweeteners, dyes or preservatives, and will not stain the teeth.
For other easy ways to improve your breath, see our previous post.
Image by twenty_questions, via Flickr
Comments Off on Bad Breath? Good News!
Filed under Oral Health, Oral Hygiene
Smart & Safe Dental X-Rays
 About a year ago, researchers established a possible link between routine dental x-rays and cancer (intracranial meningioma in particular) – more reason why, as we mentioned, x-rays in our office are never “routine.”
About a year ago, researchers established a possible link between routine dental x-rays and cancer (intracranial meningioma in particular) – more reason why, as we mentioned, x-rays in our office are never “routine.”
Since then, there have been more studies – and ongoing debate about what the research means for dentists. The latest is a paper in the Annals of Oncology, which ultimately gives a more nuanced view. While the relation between brain tumors and x-ray frequency persists, a key difference was found.
According to the study authors, “multivariable unconditional logistic regression analysis showed that the risk of BBT [benign brain tumor] increases as the frequency of received dental diagnostic x-ray increases.” However, they found no significant association between malignant brain tumors and dental diagnostic x-ray exposure.
The study abstract is available here.
For a long time, ADA recommendations were just for a full mouth series of x-rays for first time patients, then bitewings at intervals ranging from every 6 months to every 3 years, depending on the patient’s age and risk of decay or gum disease. Late last year, however, they updated their guidelines, saying that
dental X-rays help dentists evaluate and diagnose oral diseases and conditions, but the ADA recommends that dentists weigh the benefits of taking dental X-rays against the possible risk of exposing patients to the radiation from X-rays, the effects of which can accumulate from multiple sources over time.
And we think that’s as it should be: patient health and safety first. It’s why our office practices mercury-free, mercury-safe dentistry. It’s why we insist on using only biocompatible materials. And it’s why we use digital imaging, which lowers radiation exposure by as much as 90% while offering superior quality, and only take them when needed for an accurate diagnosis.
For x-rays remain an important diagnostic tool, letting us see what the naked eye cannot – inside the tooth and gums – so problems can be identified (or ruled out) and a plan of action made to solve them efficiently and safely.
Image via Medgadget
Comments Off on Smart & Safe Dental X-Rays
Filed under Dentistry, General Health
“Gluten-Free” Doesn’t Have to Mean “Low Fiber”
Commenting on last month’s post about whole grains, a reader raised an issue that’s often overlooked: How to get enough fiber when eating gluten-free. “I’ve been looking for more fiber in foods,” she wrote, “and find that often, but not always, whole grain labeled foods have more of it.” Gluten-free choices, she added, “typically have little fiber in them.”
And that’s true – but only insofar as you think of grains as your main source of fiber. Gluten and fiber, however, do not go hand in hand.
Unlike gluten – a protein composite – fiber isn’t a nutrient. It’s the part of edible plants that we can’t digest (“roughage”), yet it affects how nutrients are absorbed and the composition of gut flora. Most known for promoting regular bowel movements (keeping a person “regular”), it’s also been shown to lower cholesterol, normalize blood glucose and insulin levels, and reduce risk of some cancers.
Only some edible plants contain gluten, but all contain fiber. This leaves you with an incredibly diverse selection of foods!
 Rather than looking for gluten-free grain-based products, look to fresh vegetables and fruits, as well as legumes (beans, peas), nuts and seeds.
Rather than looking for gluten-free grain-based products, look to fresh vegetables and fruits, as well as legumes (beans, peas), nuts and seeds.
Eating a wide variety of these foods can ensure a healthy fiber intake (a minimum of 25 grams daily is generally recommended). Some, of course, deliver more fiber than others. One serving of white beans, for instance, gives you almost a whole day’s worth: 19 grams! Individual vegetables and fruits can range from 2 or 3 grams per serving to more than 10. Mix a variety together with salad greens, and again, you’ve met a good part of the recommended daily intake.
You can learn much more about these gluten-free, high-fiber foods here.
When you have any kind of food sensitivity that makes you define your diet by what you can’t have, it can be all too easy to overlook the wealth of things you can. Focusing more on the latter, you may find yourself depending less on finding analogs to replace foods you miss – gluten-free bread or pasta, for instance – and enjoying the adventure of discovering new foods you like and that deliver the nutrition you need.
Image by 365 Dias que Acalmaram o Mundo, via Flickr
Comments Off on “Gluten-Free” Doesn’t Have to Mean “Low Fiber”
Filed under Diet & Nutrition
Trees, Green Spaces & Your Health
 Have you ever wondered why it can feel so good to be among the fresh air and greenery of the great outdoors? According to a new study, there seems to be a distinctive link between trees and human health. And a small beetle showed the way.
Have you ever wondered why it can feel so good to be among the fresh air and greenery of the great outdoors? According to a new study, there seems to be a distinctive link between trees and human health. And a small beetle showed the way.
Inadvertently brought to North America from its native Asia around the turn of the century, the emerald ash borer has devastated the ash tree population of the upper Midwest in particular. All 22 species of ash are vulnerable to it, and it almost always ends up killing the trees. More than 100 million have thus far.
How might this loss affect us? Researchers looked at data from 15 states across a 17 year span, including several years before the borer was introduced. What they found was an increase in human deaths from cardiovascular and lower-tract respiratory diseases. The greater the tree loss, the greater the increase in mortality. Said lead author Geoffrey Donovan,
“There’s a natural tendency to see our findings and conclude that, surely, the higher mortality rates are because of some confounding variable, like income or education, and not the loss of trees…. But we saw the same pattern repeated over and over in counties with very different demographic makeups.”
The findings were published in the American Journal of Preventive Medicine.
And they follow numerous other studies that likewise demonstrated a strong relationship between nature and human health. Among the earlier research mentioned in The Atlantic’s coverage of the new study: a 2010 paper that
looked at the presence of parks and forests in the vicinity of people’s homes and their ability to act as a “buffer” against stress. [Its authors found] that the presence of “green space” was more closely related to physical – in terms of minor complaints and perceived general health – than mental well-being.
Other research has shown that obesity is less of a problem for children in greener neighborhoods, and those diagnosed with ADD/ADHD show marked symptom improvement after spending time in natural settings. College students with dorms that look out on nature tend to score higher on attention tests. Girls who live in homes with greener views show enhanced concentration and self-discipline, academic improvement and more thoughtful decision-making.
Here are some of the other health benefits that have been shown to come with the (green) territory:
- Increased physical fitness
- Lower stress and anxiety
- Improvements in blood pressure and muscle tension
- UV protection
- Relief from eye strain
- Less aggravation of allergies (due to tree-filtered air)
- Faster healing and recovery rates
Of course, trees are great for the health of our environment, as well. (Let canopy.org count the ways…)
Environmental health. Our health. A virtuous circle.
Maybe that new ash tree study is just the kind of wake-up call we need to accept the connectedness of all life. The call to environmental stewardship is not just a noble one. It’s a call we must answer for the sake of our own health and well-being.
Image © Dane Jessie
Filed under General Health, Holistic Health


You must be logged in to post a comment.